- Visibility 12 Views
- Downloads 3 Downloads
- DOI 10.18231/j.idjsr.2022.015
-
CrossMark
- Citation
CTOR plates- Revolutionizing treatment of complex malocclusions
- Author Details:
-
Vinay Dua *
-
Amandeep Kaur
Introduction
The success of orthodontic treatment lays its back on deriving anchorage to treat malocclusions.[1] The use of extraoral anchorage devices such as headgears, facemasks require full patient cooperation, which is sometimes not possible and is unpredictable. However, introduction of implants in orthodontics have solved this problem. In 1990s, orthodontic anchorage devices, such as miniscrews and mini-plates, were developed and these devices have been well accepted all over the world. Often called temporary anchorage devices (TADs), they have become one of the best sources of reliable anchorage and have revolutionized the field of anchorage in orthodontics, easing out the tedious mechanics that were previously used.[2]
TADs are marred by drawbacks of causing soft tissue and hard tissue complications, complexity of placement at ideal position, loading of implants and difficult removal if partial osseointegration has occurred and general systemic risk factors.[3] As TADs require adequate bone structure i.e., Cortical bone for their action, the most common problem encountered is the surrounding bone resorption due to which TAD failure occurs, often seen as screw fracture or loosening of screws.[4], [5] Newer sites for placement like the zygomatic buttress, the buccal cortical plate does provide an alternative but affect the clinician’s dexterity to operate them. Associated emphysema, nerve injury and peri implantitis also counts as an additive risk.[6] There is evidence suggesting that torsional stresses cause microfractures in surrounding bone.[7]
The forces and moments generated on TADs are challenging and often two couple systems are not preferred.[8] Complex mechanics do not go hand in hand with these anchorage units. Multiple placement of TADs also poses patient discomfort[9] and adds to the overall cost of the treatment. For this reason, many clinicians came up with the idea of placing plates by raising the flap and deriving bone anchorage for applying orthopedic forces. These plates were thus. placed via surgical procedure assisted by TADs, required another specialist, also making it a more expensive option. These plates were not versatile and their shape and size was not compatible to applied mechanotherapy. Also, these are difficult to place and remove, so they could never become a part of mainstream orthodontics.
The CTOR plates were developed by Consortium for Translational Orthodontics Research[1] www.orthodonticscientist.organd PSM (PSM North America Inc, Germany, www.psm.ms) offers a great clinical advantage to overcome these problems.[1]
Increase stability of TADs.
Increase accessibility.
Increase operability.
Decrease complications (Hard and soft tissue) as no surgical procedure is required i.e. raising of flaps.
Cost-effective.
Application of forces and moments needed for both orthopedic and orthodontic forces.
Adaptable and modifiable as per required mechanics.
Installation
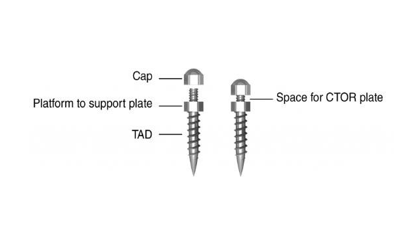
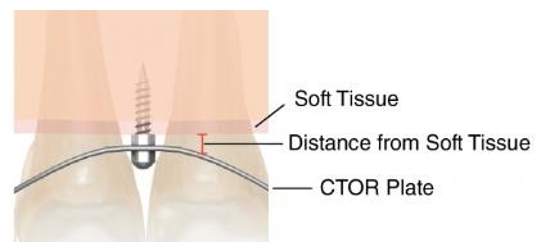
It uses minimum two TADs placed with the help of conventional miniimplant driver in order to increase the contact area for more stronger support for anchorage from the cortical bone. These TADs have a specially designed platform to support the plate, with a cylindrical hole with proper thread ([Figure 1]).[1] The plate is secured by placing the screw on cap. Placement is at least 1mm away from the soft tissue so as to prevent irritation ([Figure 2]). The plate has an implant leeway space (1-6mm) to allow flexibility based on bone quality, accessibility and anatomic restrictions ([Figure 3]). Modification of any kind may be done just by unscrewing the TADs and placing it again.


The different designs and clinical consideration
Anterior plate (A-plate)
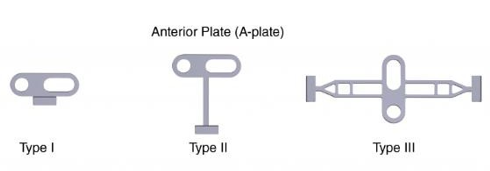
TADs have a major drawback that they cannot apply vertical forces efficiently and often the stresses and moments produced lead to loosening or unscrewing of the implants,[10], [11], [12] For this problem the A-plates are designed that help in intrusion or extrusion of the anterior teeth without altering the posterior tooth positions.[1] These are extremely helpful in open -bite and deep – bite cases.[1] They are of 3 types ([Figure 4])
Type I and Type II – for buccal placement
Type III – for palatal use
A tube is connected to the A-plate that ferments unidirectional forces, easily handled by the placement of implants and thus reducing the need for fixed appliances to correct these malocclusions ([Figure 5]).
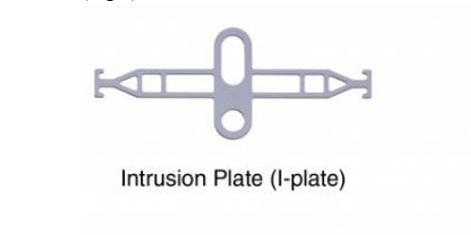
Intrusion plate (I-PLATE)
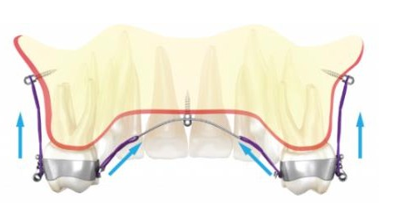
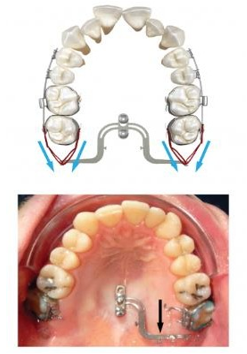
It is an easy and convenient solution for intrusion of posterior maxillary segment for treating severe open bite, Skeletal Class II malocclusion or after expansion of the maxilla in Class III patients. It is kept in place with the help of buccal TADs and is connected with the help of power chains or E-Chains for intrusion ([Figure 6]). The forces in action are seen with blue arrows ([Figure 7]).
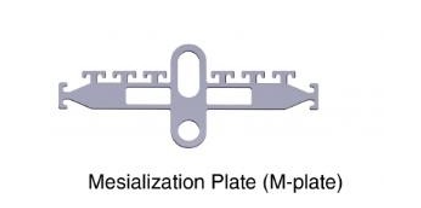
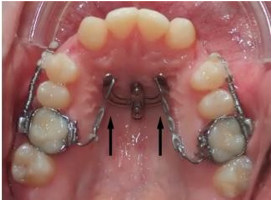
Mesialization plate (M-PLATE)
They are designed to mesialize the maxillary posterior segment or anterior segment, bilaterally or unilaterally by placing them on the palate.[1] Unilateral movement can take place by removing one wing of the plate. The plate can be rotated by 180 degrees for retraction purpose. It comes with multiple hooks ([Figure 8]) for easing the force application along the center of resistance of the teeth involved, thus helpful when patients want to avoid braces in the anterior teeth and protraction of anterior segment is required. With the mesialization plate there is significant increase in anchorage when it is jeopardized in complex cases. It is also successful in space closure where anterior segment does not need retraction, molars act as anchor units by being stabilised by the M-plate and canines, premolars are protracted.[1] ([Figure 9]).
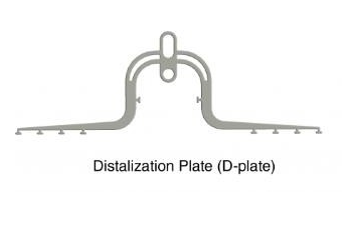
Distalization plate (D-plate)
In several cases like Class II malocclusion we may require distalizing the posterior segment of maxilla or in cases of excessive crowding where distalization provides us sufficient space to resolve the problem, the D-plates are helpful in bilateral or unilateral distalization of posterior maxillary teeth ([Figure 10]). [1] In cases of missing molar or premolar the distalizing plate helps to close the space and simultaneous retraction. It applies a simultaneous lingual and buccal force to the target teeth given by blue and black arrows ([Figure 11]).
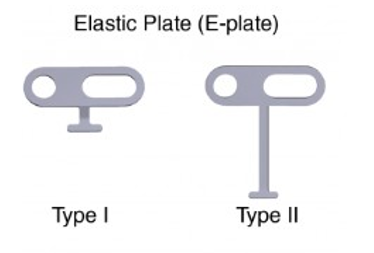
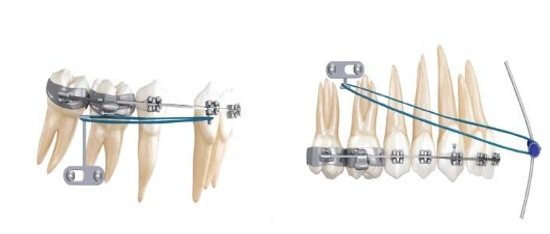
Elastic plate (E-plate)
E plate is a versatile option for retraction, protraction, intrusion and extrusion of anterior or posterior segments. It can be used in both the arches and is available in 2 forms (Type I and Type II) ([Figure 12]) which can modify the force direction and accessibility. [1] They are used in situation of Class II and Class III malocclusions where elastics are required but there are anatomic limitations and individual TADs are not sufficient for high orthopedic forces.[13]
It allows great flexibility of being able to accommodate facemask and other skeletal anchorage devices to correct skeletal discrepancies leading to complex malocclusions ([Figure 13]).[14]
Conclusion
Since there launch the CTOR plates have not only provided an innovative solution for wide spectrum of orthodontic and orthopedic problems but have also resolved the problems associated with TADs.[1] Not only it helps to increase the stability of TADs but it also helps to apply multiple forces without any surgery or need of cortical bone as such which was the prime factor why TADs still remain a complex thing.[11] As orthodontic clinicians where anchorage is of utmost importance nothing can replace the need of wanting an absolute anchorage control where CTOR plates help to nullify all the unwanted anchorage losses. The wide range of actions and force applications allows us to bring about changes in all 3 planes of space whether retraction, protraction, intrusion and extrusion. It has also been used with clear aligners as well. The ease of placement, patient comfort, cost – effectiveness and negligible side effects have given the CTOR a promising future.
Key Messages
(Provide appropriate messages of about 35-50 words to be printed in centre box):
Source of Funding
None.
Conflict of Interest
None.
Acknowledgement
The CTOR has 8 patents and 3 of them are commercially available for use
Propel Inc. developed a device based on CTOR research on micro-osteoperforations which is an uprising in accelerated orthodontics.
VPro5 – Based on mechanical stimulation of alveolar bone a patient /home care device has been launched that doubles the rate of orthodontic movement.
Robotic Ultraadaptable Braces A US patent has been given to the CTOR plates on 27 June, 2017.
References
- M Alikhani, C Sangsuwon, S Alansari, JM Nervina, SP Oliveira, CC Teixeira. CTOR Plates: A new invention for non-surgical treatment of complex malocclusions. Innovation 2021. [Google Scholar]
- D M Ramírez-Ossa, NE Correa, MAR Bustamante, A A Agudelo- Suarez. An umbrella review of the effectiveness of temporary anchorage devices and the factors that contribute to their success or failure. J Evid Based Dent Pract 2020. [Google Scholar]
- M Motoyoshi, M Inaba, A Ono, S Ueno, N Shimizu. The effect of cortical bone thickness on the stability of orthodontic mini-implants and on the stress distribution in surrounding bone. Int J Oral Maxillofac Surg 2009. [Google Scholar]
- H Mohammed, K Wafaie, MZ Rizk, M Almuzian, R Sosly, DR Bearn. Role of anatomical sites and correlated risk factors on the survival of orthodontic miniscrew implants: a systematic review and meta-analysis. Prog Orthodont 2018. [Google Scholar]
- A Costa, G Pasta, G Bergamaschi. Intraoral hard and soft tissue depths for temporary anchorage devices. Semin Orthod 2005. [Google Scholar]
- B T Brettin, N M Grosland, F Qian, K A Southard, T D Stuntz, T A Morgan, S D Marshall, T E Southard. Bicortical vs monocortical orthodontic skeletal anchorage. American Journal of Orthodontics and Dentofacial Orthopedics 2008. [Google Scholar]
- C E Misch, Z Qu, MW Bidez. Mechanical properties of trabecular bone in the human mandible: implications for dental implant treatment planning and surgical placement. J Oral Maxillofac Surg 1999. [Google Scholar]
- F Alharbi, M Almuzian, D Bearn. Miniscrews failure rate in orthodontics: systematic review and meta-analysis. Eur J Orthod 2018. [Google Scholar]
- Y G Kang, JY Kim, YJ Lee, KR Chung, YG Park. Stability of mini-screws invading the dental roots and their impact on the paradental tissues in beagles. Angle Orthod 2009. [Google Scholar]
- D Dalessandri, S Salgarello, M Dalessandri, E Lazzaroni, M Piancino, C Paganelli. Determinants for success rates of temporary anchorage devices in orthodontics: a meta-analysis (n> 50). Eur J Orthod 2014. [Google Scholar]
- Y Chen, HM Kyung, WT Zhao, WJ Yu. Critical factors for the success of orthodontic mini-implants: a systematic review. Am J Orthod Dentofac Ortho[ 2009. [Google Scholar]
- M Leo, L Cerroni, G Pasquantonio, SG Condò, R Condò. Temporary anchorage devices (TADs) in orthodontics: review of the factors that influence the clinical success rate of the mini-implants. Clin Ter 2016. [Google Scholar]
- C J Chang, WC Lin, MY Chen, HC Chang. Evaluation of total bone and cortical bone thickness of the palate for temporary anchorage device insertion. J Dent Sci 2021. [Google Scholar]
- W K Tsui, HD Chua, LK Cheung. Bone anchor systems for orthodontic application: a systematic review. Int J Oral Maxillofac Surg 2012. [Google Scholar]
